Acetone in breath analysis
Discover here a practical use case for our Acetone NDIR Gas sensor.
Acetone in breath principles
Along with acetylacetic acid and beta-hydroxybutyric acid, acetone is one of the ketone bodies found in the blood and urine. We all produce a small amount of ketones, which are then eliminated through the respiratory tract and urine. Ketones are produced naturally by the liver and are therefore present in the blood at a concentration maintained at around 1 mg/dl-1. Acetone crosses the membrane barrier and enters the pulmonary alveoli and airways due to its high vapor pressure. It is therefore found in the breath.
SCIENCE
How to measure acetone in breath with infrared spectroscopy?
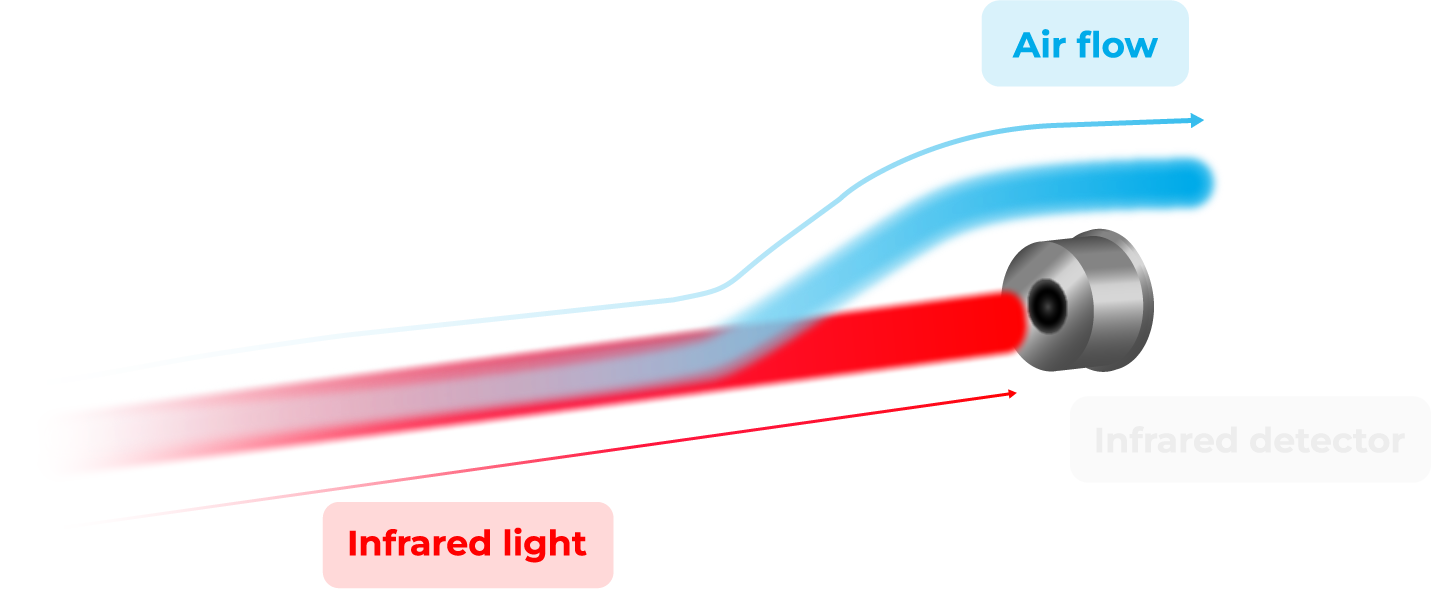
Infrared spectroscopy detection relies on an in-depth electronic analysis of the scope of a beam of infrared radiation passing through a breath sample to find the acetone concentration by identifying molecules based on how they absorb light. Using this technique, spectrometers are able to measure the amount of acetone present in the breath and display the results.
A light source emits infrared radiation, which is introduced through a measuring chamber and is finally measured by a detector. As the gas is measured in the chamber, it absorbs a part of the radiation due to molecules, reducing the intensity of the optical signal. This allows to deduce the concentration of gas.
However, more than a single compound may absorb radiation at one or more similar wavelengths to acetone, but the IR spectroscopy technology combined to algorithms is able to identify these particular compounds thanks to their signature wavelengths, and not take them into account.
Acetone, a biomarker of various disorders and diseases
Ketosis

When our body is deprived of glucose, it produces more ketone bodies to compensate for this deficiency and lack of energy: this is a state of ketosis. The body stores carbohydrates as glycogen in the liver and muscles. When there is enough glucose, the body finds its primary source of energy. However, when carbohydrate intake is significantly reduced, glycogen stores are depleted within a few days. The body then turns to a new source of energy: body fat. To get energy from fat, the body must convert it into ketones.
The term “ketosis” refers to this state where the body uses fat as fuel. Ketosis is not necessarily related to diabetes, but rather to fasting or nutritional intervention. Some people voluntarily seek this state in order to lose weight, through a ketogenic diet. Ketone levels in the blood equal to or less than 0.5 mmol/L are considered low or normal. Ketone levels between 0.5 and 3 mmol/L indicate that the body is in nutritional ketosis.
Ketoacidosis
Ketoacidosis is the pathological result of a too high level of acetone in the blood. It is characterized by an excessive production of ketone bodies by the body. The cause of ketoacidosis is mainly diabetes. Indeed, hyperglycemia due to too much sugar in the blood, related to a deficiency of insulin that allows the storage of glucose in the cells of the brain, adipose tissue, liver and muscles. Diabetes is characterized by a blood sugar level above 1.26g/L. Diabetic ketoacidosis is the most common form of ketoacidosis, but more rarely, it can also be caused by :
- A consequence of prolonged ketosis due to undernutrition, which is not eating enough or a good balance of carbohydrates. Ketone levels increase when the body is deprived of carbohydrates. This can also be the case in patients suffering from anorexia, during a weight loss diet, fasting, or because of excessive alcohol consumption leading to repeated vomiting.
- Liver pathology, the liver malfunctions and metabolizes lipids.
A normal level of acetone in the blood is usually less than 0.3 mmol/L. Above 3 mmol/L, the person has diabetic ketoacidosis. Exhaled acetone is usually between 300 and 900 ppb in healthy humans and exceeds 1800 ppb in diabetic patients.
 Acetone attacks in children
Acetone attacks in children
Acetone attacks can be frequent in children and are characterized by recurrent vomiting. Indeed, the metabolic system of the child under 10 years of age is not yet fully functional, along with a liver that is not very tolerant. Since the hepatic system is able to produce and regulate ketone bodies, it is not abnormal that, under certain conditions, the liver is not able to play its role and that acetonemia occurs.
Link between blood glucose and breath acetone
In ketosis or ketoacidosis, fats are broken down by the liver to produce two types of water-soluble ketones: acetoacetic acid and beta-hydroxybutyric acid. In addition, a third type of ketone, acetone, is also formed by further enzymatic decarboxylation of acetoacetic acid. Acetone crosses the membrane barrier and enters the pulmonary alveoli and airways due to its high vapor pressure and so it is typically found in breath.
Therefore, the analysis of exhaled acetone is recognized as an additional tool for the diagnosis and monitoring of diabetes, particularly type 1 diabetes. It is thus essential to determine the corelation between the concentration of exhaled acetone and blood glucose. Two correlation patterns exist, both in diabetic and healthy individuals:
- People whose correlation between blood glucose and exhaled acetone is linear (most common).
- People whose correlation is inverse, i.e., as blood glucose increases, breath acetone decreases.
Hense, it is necessary to determine the correlation between blood glucose concentrations and, under different conditions, for example, insulin levels, and also to correlate the results with clinical tests, for example, Hb1Ac (glycated hemoglobin).
Sources
- Saasa V, Malwela T, Beukes M, Mokgotho M, Liu CP, Mwakikunga B. Sensing Technologies for Detection of Acetone in Human Breath for Diabetes Diagnosis and Monitoring. Diagnostics (Basel). 2018 Jan 31;8(1):12. doi: 10.3390/diagnostics8010012. PMID: 29385067; PMCID: PMC5871995.
- Rydosz A. A Negative Correlation Between Blood Glucose and Acetone Measured in Healthy and Type 1 Diabetes Mellitus Patient Breath. J Diabetes Sci Technol. 2015 Jul;9(4):881-4. doi: 10.1177/1932296815572366. Epub 2015 Feb 17. PMID: 25691653; PMCID: PMC4525665.
- Gus Hancock et al 2021 J. Breath Res. 15 017101
